Diverticulosis
Comprehensive Guide
Diverticular Disease: A Comprehensive Overview
Definition
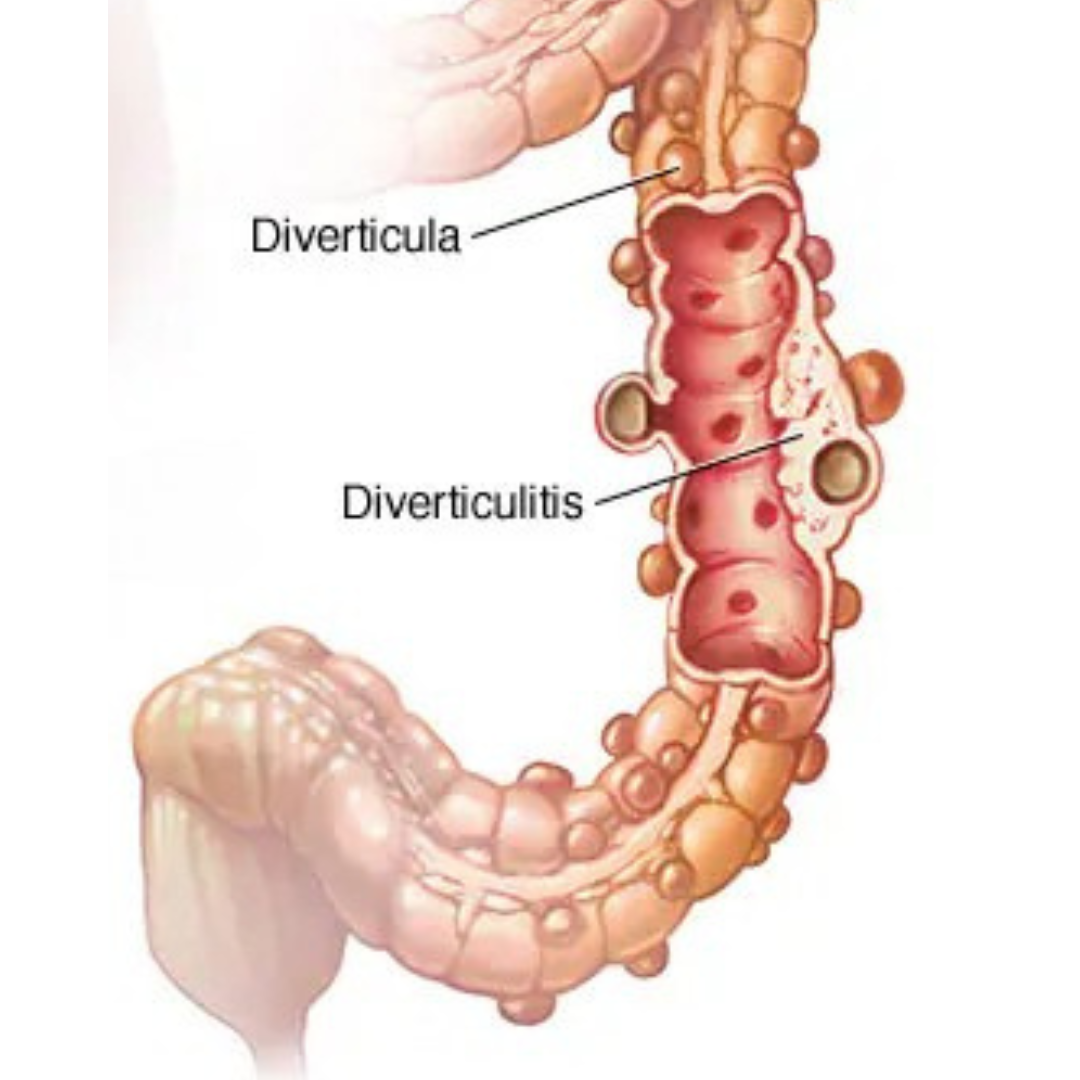
Diverticular disease encompasses conditions involving diverticula, saclike mucosal pouches in the gastrointestinal (GI) tract. Diverticulosis refers to the presence of diverticula, while diverticulitis is the inflammation or infection of a diverticulum. Diverticula are classified as true (involving all GI wall layers, e.g., Meckel’s diverticulum) or false (pseudodiverticula, involving only mucosa and submucosa, e.g., colonic diverticula).
Causes
Diverticula form due to increased intraluminal pressure, pushing mucosa through weak points in the bowel wall. Risk factors include low-fiber diets, obesity, sedentary lifestyles, smoking, and use of NSAIDs. Genetic predisposition and alterations in colonic wall structure also play a role.
Symptoms
• Diverticulosis: Typically asymptomatic but may cause bloating, abdominal pain, or constipation (symptomatic uncomplicated diverticular disease, SUDD).
• Diverticulitis: Left lower abdominal pain, fever, nausea, and possible complications such as abscess, fistula, or bowel obstruction.
• Diverticular bleeding: Painless rectal bleeding, often brisk and originating from the proximal colon.
Complications
• Diverticulitis: Can lead to abscess, perforation, or fistula.
• Diverticular bleeding: The most common cause of lower GI bleeding in adults.
• Segmental Colitis Associated with Diverticulosis (SCAD): Chronic colonic inflammation linked to diverticulosis.
Diagnosis
• Diverticulosis: Often incidental, identified via colonoscopy, CT, or barium enema.
• Diverticulitis: Diagnosed with CT imaging, possibly with ultrasound. Colonoscopy is recommended after resolution to rule out malignancy.
• Diverticular bleeding: Colonoscopy is key, with CT angiography or radionuclide imaging for ongoing bleeding.
Treatment
• Asymptomatic Diverticulosis: No treatment needed.
• Diverticulitis: Managed based on severity; uncomplicated cases may not require antibiotics. Severe cases may need hospitalization, IV fluids, or surgical intervention for complications.
• Diverticular Bleeding: Often resolves spontaneously, but endoscopic or angiographic intervention may be necessary. Surgery is reserved for refractory cases.
• SCAD: Treated symptomatically with antibiotics, 5-aminosalicylic acid, or corticosteroids for refractory cases.
Prevention
High-fiber diets, regular exercise, and avoiding NSAIDs may reduce the risk of diverticulitis. Nuts, seeds, and popcorn are no longer considered risk factors.
Key Takeaway
Diverticular disease is common, particularly with age, and often asymptomatic. Prompt diagnosis and tailored treatment are essential to managing complications like diverticulitis and bleeding.