Colonic Diverticulitis
Comprehensive Guide
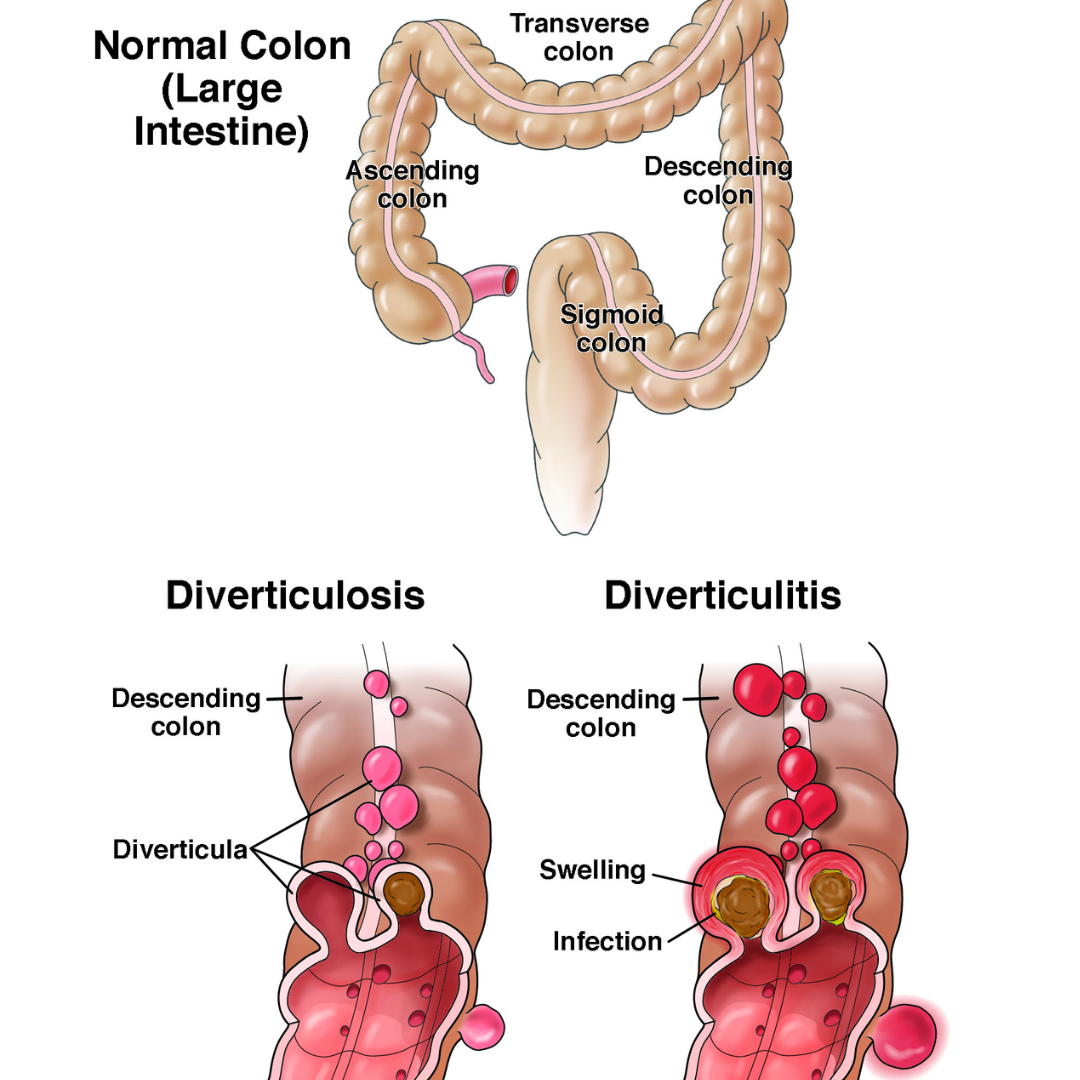
Definition
Colonic diverticulitis is the inflammation, with or without infection, of a colonic diverticulum. It can result in complications like bowel wall phlegmon, peritonitis, perforation, abscess, or fistulas. It primarily presents as abdominal pain and is diagnosed using CT or ultrasound. Treatment includes bowel rest, antibiotics, and sometimes surgery.
Etiology
Diverticulitis is believed to occur when micro or macro perforations develop in a diverticulum, releasing bacteria and triggering inflammation. Cytomegalovirus and other inflammatory factors may also contribute. Risk factors include:
• High red meat consumption
• Smoking and obesity
• NSAIDs, aspirin, corticosteroids, and opioids
• Low dietary fiber and sedentary lifestyles
Classification
1. Acute Uncomplicated Diverticulitis: Most common, with localized inflammation.
2. Acute Complicated Diverticulitis: Involves abscesses, fistulas, bowel obstruction, or free perforation.
3. Chronic Diverticulitis: Ongoing symptoms with or without complications.
Symptoms
• Left lower quadrant abdominal pain (or right-sided pain in Asian populations)
• Fever, nausea, vomiting, and bowel changes
• Severe cases may include signs of peritonitis, fistulas, or bowel obstruction
Diagnosis
1. Imaging:
• CT of the abdomen and pelvis is the primary diagnostic tool.
• Ultrasound can be used but is less reliable for complicated cases.
2. Colonoscopy:
• Recommended 1-3 months post-resolution to exclude malignancy.
Treatment
1. Uncomplicated Diverticulitis:
• Bowel rest with a clear liquid diet for 2-3 days.
• Antibiotics are considered case-by-case.
2. Complicated Diverticulitis:
• Abscess: CT-guided or ultrasound-guided drainage for abscesses >3 cm.
• Surgery: Required for free perforation, persistent abscess, or severe symptoms.
• Procedures include segmental colectomy with anastomosis or temporary colostomy.
3. Recurrent Cases:
• Evaluate surgery based on individual risk and recurrence patterns.
Complications
• Abscess formation (15% of complicated cases)
• Fistulas, bowel obstruction, and peritonitis
• Segmental colitis associated with diverticulosis (SCAD)
Prevention
• High-fiber diets, regular physical activity, and reduced red meat consumption
• Avoid unnecessary use of NSAIDs and opioids
Key Points
• Acute diverticulitis may recur in up to 39% of patients, with chronic symptoms in some.
• Proper diagnosis and personalized treatment are crucial for preventing complications.
• Non-surgical management is effective for most uncomplicated cases, while surgery is reserved for severe or refractory complications.