Gastroenteritis - General Overview
Overview of Gastroenteritis
Gastroenteritis is the inflammation of the stomach, small intestines, and large intestines. It is commonly caused by infectious agents but can also occur after exposure to certain drugs, medications, or toxins. Transmission pathways include foodborne, waterborne, person-to-person, or zoonotic spread. Symptoms generally include nausea, vomiting, diarrhea, abdominal cramps, and anorexia. Diagnosis is often clinical but can involve stool testing, including polymerase chain reaction (PCR) assays and immunoassays. Treatment is typically supportive, though certain bacterial or parasitic infections may require antimicrobial therapy.
In most cases, gastroenteritis is self-limiting, but complications can occur in vulnerable populations, such as young children, older adults, or those with immunocompromised conditions. Globally, gastroenteritis remains a significant health issue, with an estimated 1.6 million deaths annually, although mortality has decreased due to improvements in sanitation and oral rehydration therapy.
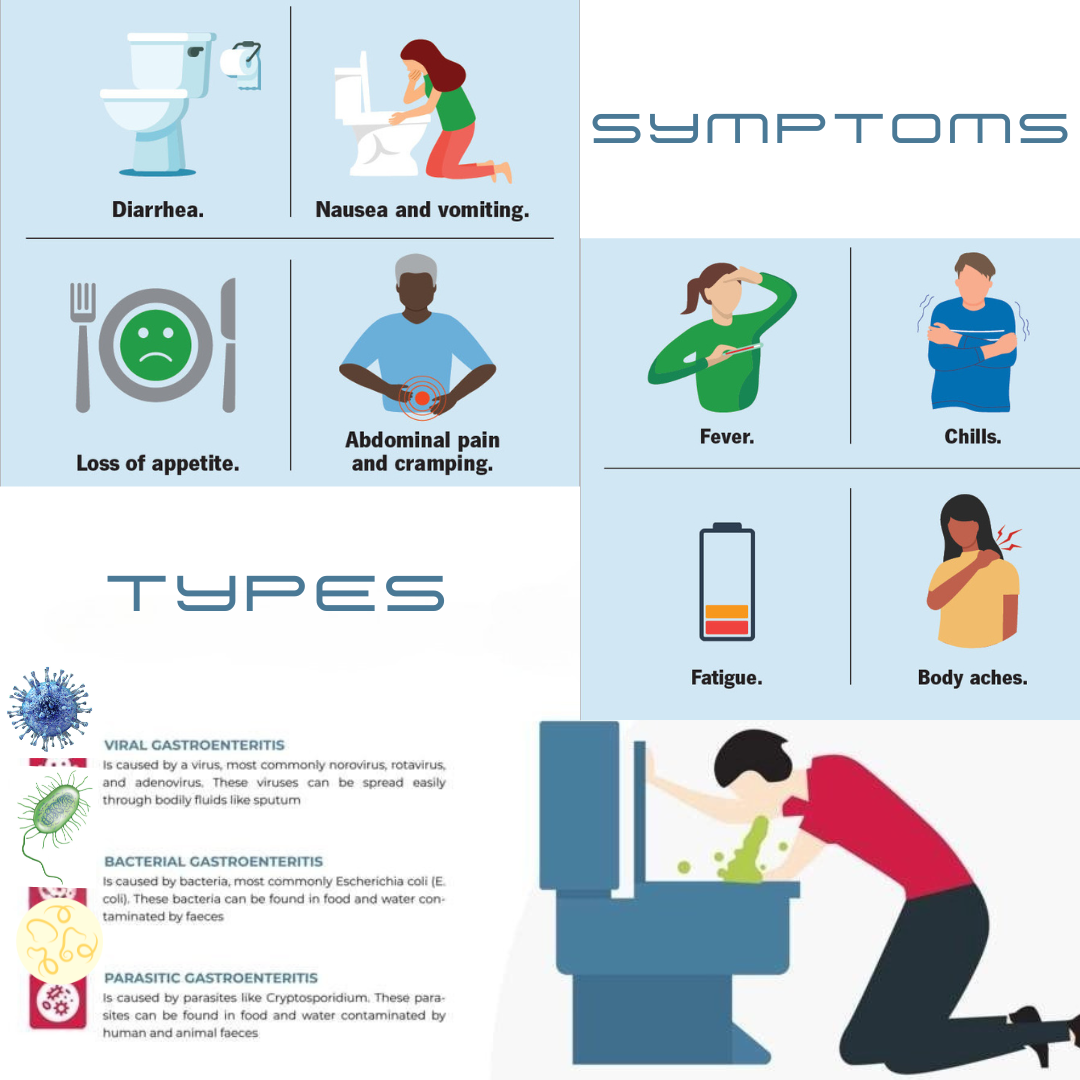
Causes of Gastroenteritis
Gastroenteritis can result from viral, bacterial, or parasitic infections. Other causes include ingestion of irritants like heavy metals or chemical toxins.
Viral Causes
Viruses are the most common cause of gastroenteritis, with norovirus and rotavirus being the primary culprits in the United States. Other common viruses include:
• Astrovirus: Typically affects infants and young children, spreading via the fecal-oral route.
• Adenovirus: The fourth most common viral cause in children under two, often accompanied by mild respiratory symptoms.
Viral infections primarily cause watery diarrhea and rarely result in inflammatory diarrhea with blood or white blood cells (WBCs). Immunocompromised individuals may experience severe symptoms from additional viruses like cytomegalovirus.
Bacterial Causes:
Bacterial gastroenteritis is less common but often more severe. Common bacteria include:
• Campylobacter and Salmonella: Frequently linked to undercooked poultry or unpasteurized milk.
• Clostridioides difficile (C. difficile): A leading cause of bacterial gastroenteritis in the U.S., particularly after antibiotic use.
• Escherichia coli (E. coli O157:H7): Known for causing bloody diarrhea and hemolytic-uremic syndrome.
• Shigella: Typically spread person-to-person but also associated with foodborne outbreaks.
Parasitic Causes
Parasites like Giardia intestinalis and Cryptosporidium parvum are the leading causes of parasitic gastroenteritis.• Giardia: Causes chronic diarrhea and malabsorption, often transmitted through contaminated water.• Cryptosporidium: Common in recreational waterborne outbreaks and highly resistant to chlorine disinfection.
Less common parasites include Cyclospora cayetanensis, Entamoeba histolytica, and Cystoisospora belli.
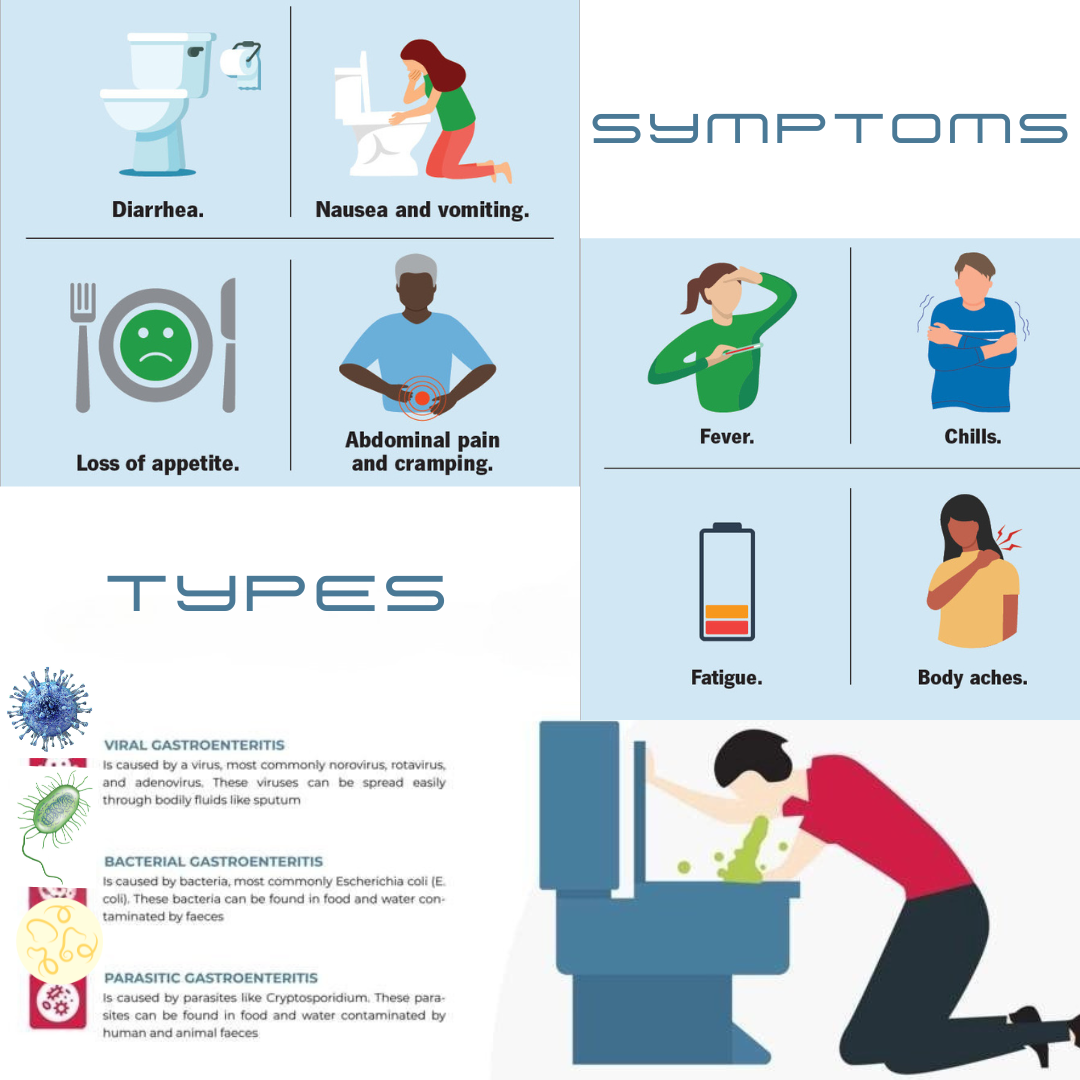
Symptoms and Clinical Presentation
Symptoms of gastroenteritis can vary based on the causative agent but typically include:
• Nausea, vomiting, and diarrhea: These symptoms often appear suddenly.
• Abdominal cramps and distension: Can range from mild to severe.
• Dehydration signs: Hypotension, tachycardia, dry mucous membranes, and reduced urine output may occur in severe cases.
• Fever: More common in bacterial or parasitic infections.
• Watery or bloody diarrhea: Viral infections usually cause watery diarrhea, while bacterial infections like E. coli O157:H7 or Shigella often lead to bloody diarrhea.
Diagnosis
Diagnosis of gastroenteritis is primarily clinical but may involve targeted tests for specific pathogens based on the patient’s history and symptoms.
1. Clinical Features:
• Sudden onset of diarrhea with or without fever or vomiting.
• Recent ingestion of contaminated food, travel history, or exposure to infected individuals.
2. Stool Testing:
• PCR Testing: Used to identify specific pathogens in severe or prolonged cases.
• Microscopic Examination: For parasites in chronic or subacute diarrhea.
• Culture: Essential for bacterial pathogens like Salmonella or Shigella.
3. Blood Tests:
• Electrolyte levels to assess dehydration.
• Complete blood count (CBC) for signs of infection or eosinophilia (indicative of parasitic infections).
Treatment
Treatment focuses on symptom management, hydration, and, in specific cases, antimicrobial therapy.
1. Supportive Care
• Rehydration: Oral glucose-electrolyte solutions or intravenous fluids in severe cases.
• Diet: Gradual reintroduction of food; no evidence supports restricting to bland diets.
• Antidiarrheal Agents: Effective for watery diarrhea in adults but contraindicated in pediatric cases and infections like E. coli O157:H7 or C. difficile.
2. Antimicrobials
• C. difficile: Treated with oral vancomycin or fidaxomicin.
• Giardia: Treated with metronidazole or nitazoxanide.
• Cryptosporidium: Nitazoxanide may be used in immunocompromised patients.
3. Probiotics
Probiotics may help restore gut flora, especially after antibiotic-associated diarrhea.
Prevention
Preventive measures include improving hygiene, food safety, and vaccination where applicable.
• Rotavirus Vaccination: An essential part of infant immunization schedules.
• Handwashing: Particularly after handling food or changing diapers.
• Safe Food Practices: Avoiding undercooked poultry, eggs, and unpasteurized milk.
• Breastfeeding: Provides protective immunity to infants.
• Water Safety: Avoid swallowing pool or recreational water; boil untreated drinking water during travel.
Key Points to Remember
1. Gastroenteritis is commonly self-limiting but can lead to severe complications in vulnerable populations.
2. Viral infections are the leading cause, followed by bacterial and parasitic infections.
3. Most cases require supportive care, with antibiotics reserved for select bacterial infections.
4. Prevention through vaccines, hygiene, and safe food practices is crucial to reducing incidence and mortality.
For more detailed management and symptom tracking, consult our app, which provides personalized recommendations and access to healthcare professionals. Take charge of your health and seek timely care when needed.
References:
1. Centers for Disease Control and Prevention: Foodborne Germs and Illnesses (2023).
2. GBD 2016 Diarrhoeal Disease Collaborators: Global Burden of Disease Study (2016).
3. Torres-Miranda D, et al: Use of BioFire FilmArray gastrointestinal PCR panel (2020).
4. Johnson S, et al: Clinical Practice Guidelines for C. difficile Infection (2021).